Doença Carotídea
SUMÁRIO
Diferença entre AIT e AVC
- O Ataque Isquêmico Transitório (AIT) é uma alteração temporária da função cerebral que dura menos de 24 horas.
- O Acidente Vascular Cerebral (AVC) tem déficits que não se revertem dentro desse período.
Causas do AVC
- 25%: Ateroembolismo de grandes vasos (incluindo as artérias carótidas).
- 25%: Doenças de pequenos vasos intracranianos.
- 20%: Embolismo de origem cardíaca.
- 5%: Causas indefinidas.
- 25%: Causas desconhecidas.
Embolização Arterial
Trombos e detritos de placas ateroscleróticas podem migrar e obstruir os vasos intracranianos, causando sintomas.
Sintomas
Os sintomas dependem da localização da obstrução e da função cerebral afetada. As artérias mais comumente obstruídas são:
- Artéria Cerebral Anterior: Irriga a superfície medial do lobo frontal, porção anterior dos gânglios da base e cápsula interna. A isquemia causa fraqueza nas pernas, perda sensorial e apatia.
- Artéria Cerebral Média: Irriga a superfície lateral do cérebro, podendo causar hemiplegia, hemianopsia, afasia e dispraxia.
- Embolização para a artéria da retina pode levar à amaurose fugaz, ocorrendo sempre no mesmo lado da lesão carotídea.
Sintomas como tontura, pré-síncope, convulsões e sintomas neurológicos periféricos não são atribuídos às artérias carótidas.
Diagnóstico e Rastreamento
- Ultrassonografia: Principal método de rastreamento, com alta sensibilidade e especificidade.
- Critérios de risco: Pacientes acima de 65 anos com dois ou mais fatores de risco devem ser rastreados.
- Índice Intimal-Médio: Um valor acima de 1,5 indica a presença de placas.
Angiografia
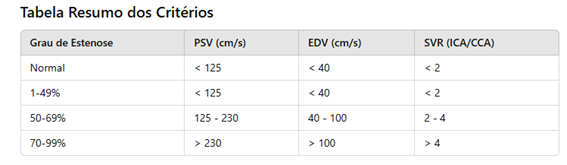
A angiografia é o padrão-ouro para o diagnóstico. Existem dois métodos principais para medir a estenose carotídea:
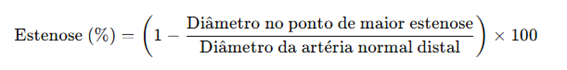
- Método NASCET: Compara o diâmetro da estenose com o segmento normal da artéria distal.
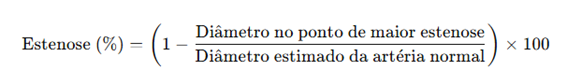
- Método ECST: Compara o diâmetro da estenose com uma estimativa do diâmetro original da artéria.
Comparando os métodos:
- O NASCET tende a calcular uma estenose menor.
- O ECST tende a calcular uma estenose maior.
Exemplo: Se a estenose mede 2 mm, o diâmetro normal distal é 6 mm e o diâmetro original estimado é 8 mm:
- NASCET = 67% de estenose.
- ECST = 75% de estenose.
Tratamento Clínico
Para todos os pacientes com aterosclerose carotídea:
- Pressão arterial <140/90 mmHg.
- Controle do diabetes (HbA1c <7%).
- Cessar tabagismo.
- Praticar atividade física.
- Reduzir o consumo de álcool.
- Controlar dislipidemia (LDL <70 mg/dL).
- Uso de AAS 100 mg/dia e estatinas de alta potência (atorvastatina 40 mg/dia).
Indicação para Cirurgia: Assintomáticos
Considera-se assintomático quando a estenose é maior que 50%, sem eventos clínicos ou radiológicos nos últimos 6 meses.
Se a ressonância mostra uma área isquêmica associada à estenose, o paciente é considerado sintomático, mesmo sem sintomas.
Critérios que indicam maior risco de AVC em assintomáticos:
- Microembolização no Doppler transcraniano.
- Placa hipoecogêncica.
- Progressão da estenose.
- Infarto silencioso no exame de imagem.
- Reserva cerebrovascular reduzida.
- Hemorragia intraplaca.
Se indicado tratamento, a endarterectomia é preferida, salvo em pacientes de alto risco cirúrgico.
Indicação para Cirurgia: Sintomáticos
A cirurgia é indicada para estenose >50%, com preferência pela endarterectomia. Pacientes com suboclusão ou oclusão total não são candidatos à revascularização.
Procedimentos Cirúrgicos
- Anestesia: Pode ser geral ou local. A geral facilita o trabalho da equipe; a local permite avaliação neurológica imediata.
- Shunt: Indicado em casos com pressão de refluxo <45 mmHg ou oclusão contralateral.
- Uso de Patch: Recomendado para fechamento, sem consenso sobre o melhor material.
- Drenagem Cervical: Deve ser de grande calibre e removido em até 24 horas.
- Reversão da Heparina: Recomendada com protamina para evitar hematomas cervicais.
Angioplastia
Alternativa à endarterectomia se o risco de AVC ou óbito for <6%. Indicada em:
- Anatomia desfavorável.
- Pescoço hostil.
- Disfunção ventricular grave.
Complicações
Principal causa de óbito: Infarto agudo do miocárdio (IAM).
Eventos neurológicos: Segunda causa de óbito.
Hematoma cervical: Reabordagem precoce necessária.
Lesões nervosas: Hipoglosso, vago, facial (ramo mandibular), laríngeo superior e acessório podem ser afetados.